The Layers of the Vaginal Wall Explained: A Practical Guide
The Layers of the Vaginal Wall Explained: A Practical Guide
The vaginal wall is far more than just a passage—it’s a complex, layered structure designed for flexibility, protection, and support. Whether you’re curious about anatomy for personal understanding or professional interest, learning the layers of the vaginal wall helps you appreciate how this part of the body functions and adapts.
In this guide, we’ll break down the main layers, their roles, and why they matter to overall health.
Understanding the Vaginal Wall: An Overview
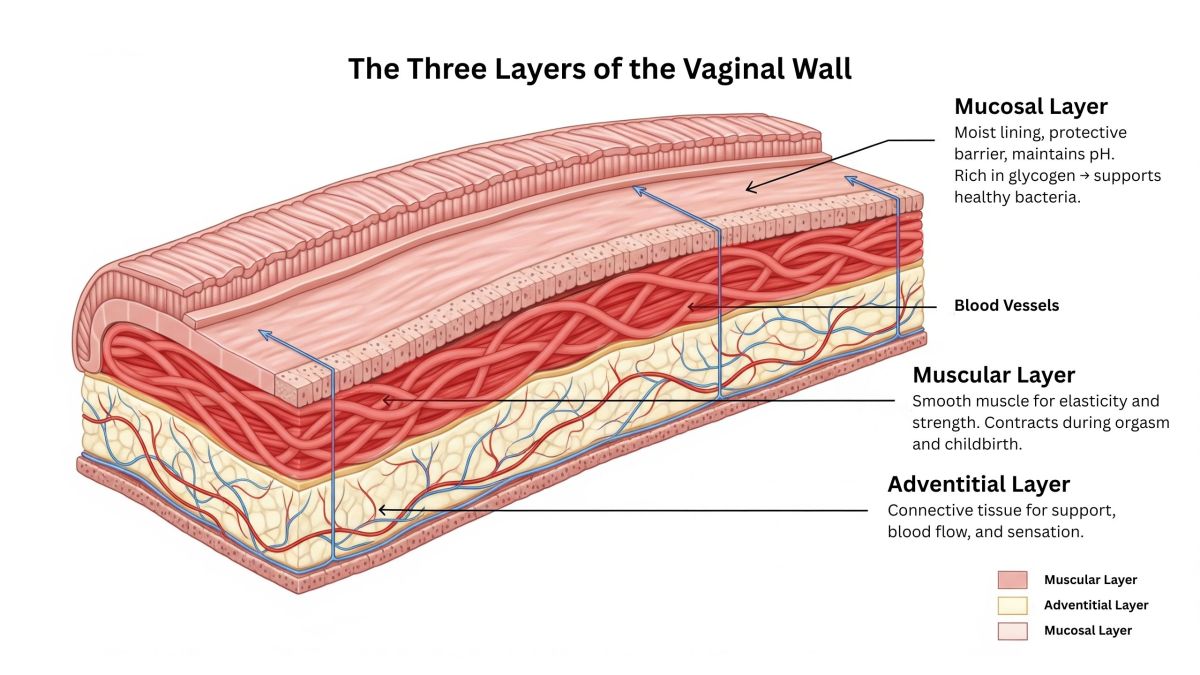
The vaginal wall is composed of three primary layers, each serving a unique function:
-
Mucosal Layer (Innermost)
-
Muscular Layer (Middle)
-
Adventitial Layer (Outer)
These layers work together to maintain elasticity, support surrounding structures, and keep the vaginal environment balanced.
1. The Mucosal Layer: The Inner Barrier
Location: The innermost surface of the vaginal wall.
Structure:
-
Made up of stratified squamous epithelium—similar to skin, but without hair follicles.
-
Rich in glycogen, which supports healthy vaginal flora.
Function:
-
Provides lubrication through transudation (moisture coming from underlying tissues).
-
Creates a protective barrier against infections by maintaining an acidic pH.
-
Responds to hormonal changes during the menstrual cycle, pregnancy, and menopause.
Why It Matters:
Disruptions to this layer—such as from antibiotics, hormonal changes, or certain infections—can lead to dryness or imbalance in the vaginal microbiome.
2. The Muscular Layer: Strength and Flexibility
Location: The middle layer, beneath the mucosa.
Structure:
-
Smooth muscle fibers arranged in circular and longitudinal layers.
-
Highly elastic to allow for expansion and contraction during sexual activity and childbirth.
Function:
-
Provides structural support.
-
Plays a role in pelvic floor stability.
-
Contracts during orgasm and childbirth.
Why It Matters:
Pelvic floor exercises like Kegels target this muscular layer, which can help maintain tone and prevent issues like incontinence or prolapse.
3. The Adventitial Layer: The Support Network
Location: The outermost layer, connecting the vagina to surrounding tissues.
Structure:
-
Dense connective tissue interwoven with blood vessels, lymphatics, and nerves.
-
Anchors the vagina to nearby organs like the bladder and rectum.
Function:
-
Provides resilience and structural integrity.
-
Houses important blood supply and nerve endings for sensation and health.
Why It Matters:
Damage to this layer, often during childbirth or surgery, can affect vaginal support and lead to pelvic floor disorders.
How the Layers Work Together
These layers aren’t isolated—they function as an integrated system. The mucosa keeps the environment balanced, the muscle provides strength and elasticity, and the adventitia ensures stability and vascular health.
Vaginal Wall Layers at a Glance
| Layer | Composition | Primary Functions | Common Changes | Care Notes |
|---|---|---|---|---|
| Mucosal (inner) | Stratified squamous epithelium; rugae; glycogen-rich | Moisture via transudate; acidic pH; microbial balance | Dryness/atrophy with low estrogen; pH shifts | Avoid douching; consider moisturizers or clinician-guided estrogen if indicated |
| Muscular (middle) | Smooth muscle—circular & longitudinal fibers | Elasticity; tone; contractions (sexual response, childbirth) | Laxity after childbirth or aging | Pelvic floor exercises; consult pelvic health physiotherapy if needed |
| Adventitial (outer) | Connective tissue with vessels, lymphatics, nerves | Support; structural integration; blood supply & sensation | Support changes after delivery or surgery | Gradual return to activity postpartum; seek care for prolapse or persistent symptoms |
Common Factors Affecting Vaginal Wall Health
-
Hormonal Changes: Menopause reduces estrogen, leading to thinning of the mucosal layer.
-
Childbirth: Can stretch and sometimes injure the muscular and adventitial layers.
-
Medical Treatments: Radiation or certain medications can alter the integrity of these tissues.
-
Lifestyle: Hydration, nutrition, and pelvic exercises support tissue health.
Tips for Supporting Vaginal Wall Integrity
-
Maintain healthy estrogen levels through diet and, if needed, medical advice.
-
Practice pelvic floor exercises to strengthen the muscular layer.
-
Avoid harsh soaps or douching, which can disrupt mucosal balance.
-
Stay hydrated and eat foods rich in collagen-building nutrients.
Final Thoughts
Understanding the layers of the vaginal wall isn’t just academic—it’s practical knowledge for maintaining comfort, function, and overall well-being. By respecting how these layers work, you can make informed choices for your health at every stage of life.
Q&A
Q1. Is the vaginal wall the same thickness for everyone?
No. Thickness varies with age, hormones, childbirth history, and individual anatomy. It can also change across the menstrual cycle.
Q2. Does the mucosal layer produce its own lubricant?
Moisture mainly comes from transudation (fluid moving through tissue). The cervix also contributes cervical mucus, which can vary during the cycle.
Q3. What maintains the vagina’s acidic pH?
Primarily lactobacilli that metabolize glycogen into lactic acid in the mucosal layer. Antibiotics, low estrogen, or infections can shift this balance.
Q4. Can Kegel exercises strengthen the vaginal wall?
They target pelvic floor muscles that coordinate with the vaginal muscular layer. Correct technique helps with support and continence, but over-tightening can cause discomfort—quality over quantity.
Q5. Why might sex feel dry or uncomfortable after menopause?
Lower estrogen can thin and dry the mucosal layer (genitourinary syndrome of menopause). Moisturizers, lubricants, and clinician-guided local estrogen are common options.
Q6. What changes after childbirth?
Temporary stretching affects the muscular and adventitial layers. Most people improve with time; pelvic health physiotherapy can help with persistent symptoms.
Q7. Are fragranced washes okay?
Gentle, unscented products around (not inside) the vulva are generally better. Avoid douching; it disrupts the mucosal balance.
Q8. Can systemic health affect the vaginal wall?
Yes—hydration, nutrition, medications, and conditions like diabetes or autoimmune disorders can impact tissue health.
Disclaimer: The articles and information provided by the Vagina Institute are for informational and educational purposes only. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or another qualified health provider with any questions you may have regarding a medical condition.


 Deutsch
Deutsch  English
English  Español
Español  Français
Français