No Test, No Sex: Why STI Checks Should Be the Standard in New Relationships

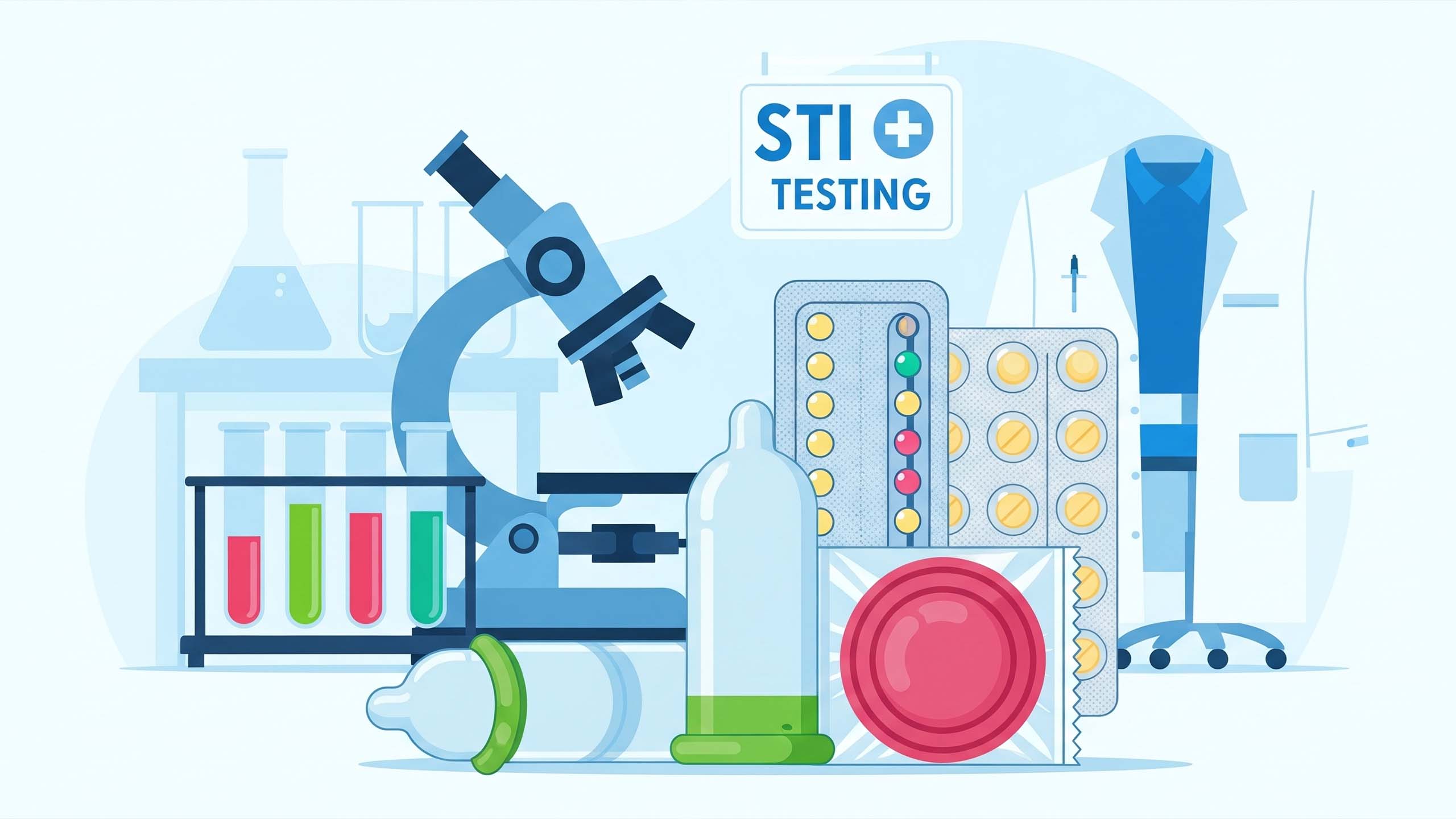
When we talk about building healthy relationships, conversations often revolve around attraction, compatibility, or emotional connection. But there’s another conversation that belongs right at the start: health. Specifically, sexual health. Before a relationship becomes sexual, one of the most important steps anyone can take is to request and share recent STI (sexually transmitted infection) test results.
This isn’t about being suspicious. It isn’t about shaming. It’s about taking your health seriously—and showing that you take your partner’s health seriously, too.
Why Asking for an STI Test Matters
The numbers alone should make us pause. Millions of new STI cases are reported worldwide every year. Many infections—including chlamydia, gonorrhea, HPV, and HIV—often show no symptoms for months, sometimes years. That means a partner could unknowingly pass something along without malicious intent.
Requesting a test is not an accusation. It’s a basic step in ensuring that intimacy is safe. Just as you wouldn’t eat at a restaurant with questionable hygiene, you shouldn’t enter a sexual relationship without clear, recent proof of your partner’s health status.
Making Testing a Non-Negotiable
The idea is simple: no test, no sex. If your partner is unwilling to get tested, that should raise questions about whether they respect your well-being. This principle, taught early and practiced consistently, could dramatically reduce the spread of infections.
Imagine if schools taught this alongside lessons on anatomy and consent. Students would grow up seeing STI tests not as a burden, but as routine. A natural part of intimacy. A step as normal as brushing your teeth before a date.
Building Trust Through Transparency
Far from creating distance, sharing test results can strengthen relationships. It shows honesty, responsibility, and respect. Partners who are open about their sexual health are more likely to communicate openly about other needs, boundaries, and expectations.
Trust doesn’t come from avoiding uncomfortable conversations—it comes from facing them head-on.
But Testing Isn’t the Only Line of Defense
Even after exchanging recent test results, protection should remain standard. Here’s why:
-
Timing matters. Some infections take weeks or months to appear on tests.
-
Risk doesn’t vanish. Just because both partners test negative today doesn’t mean future choices won’t change things.
-
Layered safety works best. Condoms, dental dams, and other protective methods lower the risk even further.
Testing plus protection isn’t paranoia—it’s prevention.
Recommended Testing & Protection Timeline
| When | What to test for | Action |
|---|---|---|
| Before first sexual contact | HIV (antibody/antigen), chlamydia, gonorrhea; consider syphilis & hepatitis per risk | Obtain results and share them; use condoms/dental dams regardless |
| 2–12 weeks after a new exposure | Repeat HIV (if within window period), chlamydia, gonorrhea | Retest if there was a potential exposure during the window period; continue protection |
| Routine / ongoing | At least annually: chlamydia, gonorrhea, HIV (more often if high-risk); HPV per local guidelines | Establish a testing schedule with partners; use protection when uncertain |
Removing the Stigma
For many people, the hardest part isn’t the test itself—it’s asking for it. Society has framed STI discussions as awkward, accusatory, or even insulting. That stigma must go.
There should be no embarrassment in wanting to protect yourself and your partner. In fact, normalizing this conversation can help rewrite what intimacy looks like. Instead of being reckless, it becomes thoughtful. Instead of secretive, it becomes transparent.
How to Bring It Up
If you’re unsure how to ask, here are some ways to phrase it without turning the moment into a confrontation:
-
“I really care about staying healthy, and I’d like us both to get tested before we have sex.”
-
“I think it’s important we share our recent test results. That way, we both feel safe.”
-
“I make it a rule to always see test results before getting intimate—it’s just part of how I take care of myself.”
Clear, calm, and confident.
A Habit Worth Keeping
Making STI testing a prerequisite isn’t about mistrust or fear—it’s about valuing life, health, and respect. It’s a habit that protects everyone, reduces disease, and can quite literally save lives.
The reality is simple: sex without protection or transparency carries risks that don’t just affect you, but also your future partners. The conversation may feel uncomfortable the first time, but with practice, it becomes second nature.
Bottom Line
Sex should be enjoyable, safe, and rooted in respect. Setting the standard of “test results first, protection always” isn’t extreme—it’s responsible. It’s a way of showing that your health, your partner’s health, and your future together matter.
Because trust isn’t built on assumptions. It’s built on honesty, action, and care.
Frequently Asked Questions
Q: What does “no test, no sex” actually mean?
It means making recent STI test results a prerequisite before engaging in sexual activity with a new partner. It’s a boundary to protect both people’s health, alongside continued use of condoms or other protections.
Q: Which tests should I ask for?
At minimum, ask about HIV, chlamydia, and gonorrhea. Depending on risk and age, include syphilis, hepatitis B/C, and HPV (where relevant). Local clinics can advise on the right panel.
Q: How recent should a test be?
Ideally within the last 3 months for many common STIs; some tests (HIV antigen/antibody) can detect infection earlier, while others have window periods—so a repeat test 2–12 weeks after potential exposure may be recommended.
Q: My partner refuses to test — what should I do?
Take their refusal seriously. You can offer to find a testing site together, suggest a joint clinic visit, or decline sex until there’s agreement. Refusal may indicate a mismatch in values about health and safety.
Q: Is sharing results safe and private?
Yes — sharing is a personal decision. Encourage secure methods (showing a clinic result in person, secure screenshot of a dated lab result, or accompanying each other to testing). Respect privacy and avoid public posting of medical records.
Q: If both partners tested negative, do we still need condoms?
Yes. Tests may miss recent infections (window period) and don’t prevent future exposures. Condoms or barrier methods remain important layers of protection.
Q: Will asking for a test offend someone?
Many people appreciate the clarity and responsibility. Use calm, matter-of-fact language (examples in the article) and frame it as mutual care rather than accusation.
Q: Should schools teach this?
Many health educators support teaching testing, consent, and protection as part of comprehensive sexual education — so young people adopt safe habits early.
Disclaimer: The articles and information provided by the Vagina Institute are for informational and educational purposes only. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or another qualified health provider with any questions you may have regarding a medical condition.


 Deutsch
Deutsch  English
English  Español
Español  Français
Français