The Four Phases of the Menstrual Cycle Explained
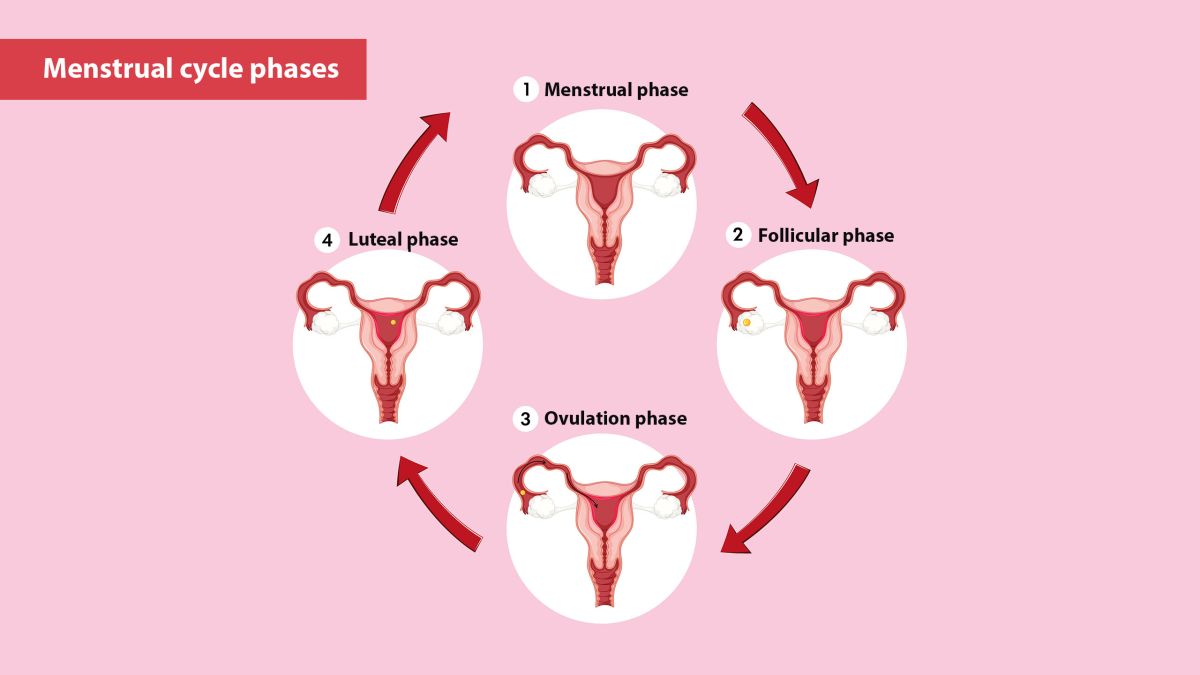
The menstrual cycle is a complex and natural process that prepares the female body for a potential pregnancy each month. This biological rhythm is regulated by hormonal changes and involves various physical and emotional shifts. Understanding the four distinct phases of the menstrual cycle helps clarify how the body functions throughout this cycle and provides insight into reproductive health.
Below is a clear explanation of each phase: what happens, why it happens, and how it may affect the body.
The Four Phases of the Menstrual Cycle
Menstrual
Days: 1–5
Hormones: Low Estrogen & Progesterone
Notes: Shedding of uterine lining; bleeding occurs.
Follicular
Days: 1–13
Hormones: Rising Estrogen, FSH
Notes: Egg matures, uterine lining rebuilds.
Ovulation
Day: Around 14
Hormones: LH Surge, Peak Estrogen
Notes: Egg released; peak fertility.
Luteal
Days: 15–28
Hormones: High Progesterone
Notes: Prepares for pregnancy; PMS may occur.
1. Menstrual Phase (Days 1–5)
The cycle begins with menstruation, commonly referred to as a period. This phase marks the shedding of the uterine lining, which had built up in the previous cycle in anticipation of a fertilized egg. When pregnancy does not occur, hormone levels—primarily estrogen and progesterone—drop, triggering the body to expel the endometrial lining.
What Happens:
-
The uterus contracts to release the lining through the vagina.
-
Blood, mucus, and tissue make up the menstrual flow.
-
This phase typically lasts between 3 to 7 days, though the length can vary.
What You Might Notice:
-
Lower energy levels.
-
Cramping or abdominal discomfort.
-
Back pain or headaches in some cases.
-
Fatigue or mood changes due to hormonal fluctuations.
Menstruation is the most visible phase of the cycle and is often the one most associated with the term “monthly cycle.”
2. Follicular Phase (Days 1–13)
The follicular phase begins simultaneously with menstruation and continues after it ends. During this time, the brain signals the pituitary gland to release follicle-stimulating hormone (FSH), which prompts the ovaries to prepare several follicles—each containing an immature egg.
What Happens:
-
Only one follicle usually becomes dominant and matures.
-
Estrogen levels begin to rise, stimulating the thickening of the uterine lining again.
-
The body prepares for potential fertilization and implantation.
What You Might Notice:
-
Gradually increasing energy.
-
More stable mood.
-
Improved concentration or alertness in some individuals.
Estrogen plays a key role during this phase, encouraging tissue growth in the uterus and promoting cervical mucus changes that assist sperm movement.
3. Ovulation Phase (Around Day 14)
Ovulation is the midpoint of the cycle. It typically occurs around day 14 in a 28-day cycle but can vary based on individual hormonal rhythms. During this phase, a surge in luteinizing hormone (LH) triggers the release of the mature egg from the dominant follicle in the ovary.
What Happens:
-
The egg travels down the fallopian tube toward the uterus.
-
It is viable for about 12 to 24 hours.
-
This is the most fertile window in the cycle.
What You Might Notice:
-
A slight rise in basal body temperature.
-
Increased libido or sensitivity.
-
Clear, stretchy cervical mucus resembling raw egg whites.
Some may also feel a mild twinge or cramp on one side of the lower abdomen, known as mittelschmerz, corresponding with the ovary that releases the egg.
4. Luteal Phase (Days 15–28)
After ovulation, the ruptured follicle transforms into the corpus luteum, which produces progesterone. This hormone helps maintain the uterine lining, preparing it to support a fertilized egg if conception occurs.
What Happens:
-
If fertilization occurs, the embryo will signal the body to continue progesterone production.
-
If not, the corpus luteum breaks down after about two weeks.
-
Progesterone and estrogen levels fall, leading to the start of menstruation again.
What You Might Notice:
-
Bloating, breast tenderness, or mood swings (common premenstrual symptoms).
-
Changes in appetite or sleep patterns.
-
A decrease in energy or concentration for some individuals.
The luteal phase remains relatively consistent in length—typically lasting about 14 days—regardless of the total cycle length.
Phase |
Typical Duration |
Key Hormones |
Common Symptoms |
Fertility Status |
|---|---|---|---|---|
| Menstrual | 3–7 days | ↓ Estrogen, ↓ Progesterone | Bleeding, cramps, fatigue | Low fertility |
| Follicular | 7–10 days | ↑ FSH, ↑ Estrogen | Increasing energy, improved mood | Low to moderate fertility |
| Ovulation | 1 day | ↑ LH surge, peak Estrogen | Higher libido, cervical mucus changes | High fertility (peak) |
| Luteal | 12–14 days | ↑ Progesterone, ↓ Estrogen | Bloating, mood swings, breast tenderness | Low fertility |
Conclusion
The menstrual cycle follows a coordinated sequence of hormonal shifts that guide the body through preparation, release, and resetting. Each phase plays a specific role in reproductive readiness and overall health. By becoming familiar with the cycle's structure, individuals can better understand changes in their physical and emotional states, track fertility, and identify potential irregularities that may warrant medical attention.
Whether for health monitoring, family planning, or general awareness, knowing the cycle's four phases—menstrual, follicular, ovulation, and luteal—offers practical insight into how the body works.
Disclaimer: The articles and information provided by the Vagina Institute are for informational and educational purposes only. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or another qualified health provider with any questions you may have regarding a medical condition.


 English
English  Deutsch
Deutsch  Español
Español  Français
Français 




